Signalment and history:
Penny is a 9.5 year old female neutered Shih Tzu. She presented with a history of 24 hours of tachpnoea and exercise intolerance triggered during a longer than normal walk. She had vomited once on the morning of presentation. The client had reported occasional coughing with exercise for a few weeks prior to presentation, and slowing on her walks for 48 hours prior to onset of clinical signs. She was not up to date with her vaccinations and her flea and worming prevention had lapsed, she was in otherwise good health.
Initial presentation and Clinical examination:
At time of initial presentation Penny was quiet but alert. Her mucous membranes were pink with a delayed capillary refill time of 2-3 seconds. Her heart rate was 120 beats per minute with a new grade IV/VI systolic murmur, with point of maximal intensity (PMI) on the right. She was tachypnoeic at 76 breaths per minute with increased effort and increased bronchial sounds. Abdominal palpation was unremarkable, and her temperature was normal.
A T-FAST was performed showing infinite B lines in all fields and a shred sign noted in the right mid chest. Left atrium to aortic ratio was measured at 1.5.

Figure 1: Lateral chest x-ray demonstrating right sided cardiac enlargement and mixed pulmonary pattern- predominantly bronchointerstitial.
What would you do next?
Initial treatment:
Penny was stabilised overnight receiving a total of 7mg /kg frusemide IV and butorphanol 0.1mg/kg IV for anxiolysis. Her respiratory rate and effort stabilised overnight to 40 breaths per minute. Her heart murmur was noted to have reduced to a grade III/VI systolic murmur. She was started on oral frusemide (Libeo) and pimobendan (Vetmedin) for suspected congestive heart failure pending echocardiography.
Further investigations:
Penny was internally referred for echocardiography which was carried out three days later. The client had noted that her breathing was much more settled and only became more tachypnoeic with exertion.
On her clinical examination she had a grade III/VI systolic heart murmur, with PMI on the right chest. Her respiratory rate was 36 breaths per minute with diffuse increased bronchial sounds with normal effort. Her mucous membranes were not assessed due to her nature.
On echocardiography, the left side of her heart was normal in appearance. There was minor mitral valve regurgitation with no significant valvular changes. The right atrium and ventricle were enlarged, and there was a large eccentric tricuspid regurgitation measuring 3.95m/s (62mmHg) consistent with pulmonary hypertension. The tricuspid valve was normal in appearance. Her main pulmonary artery was also increased in size when compared to the aorta supportive of pulmonary hypertension.
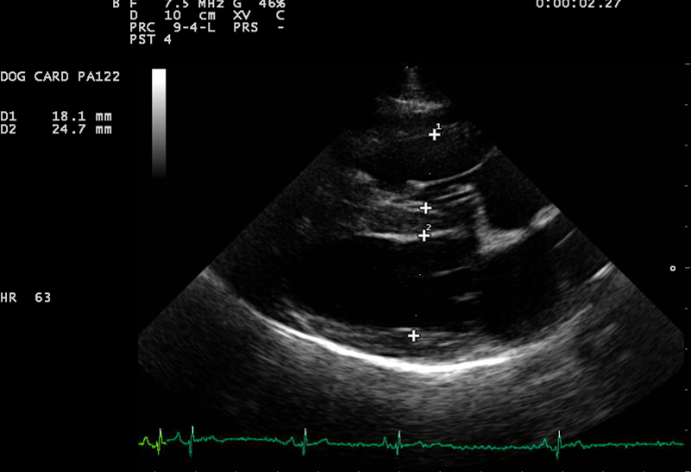
Right parasternal long axis 4-chamber view: Evidence of right ventricular enlargement. This is normally about 1/3rd to half the size of the left ventricle.
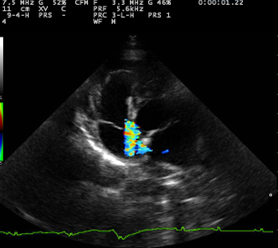
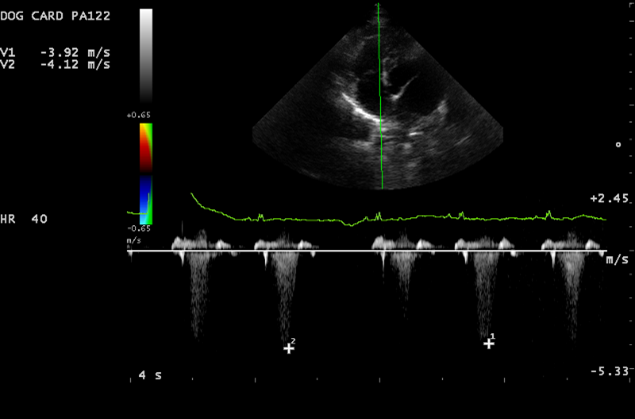
Left parasternal 4 chamber view: Tricuspid valve regurgitation and elevated tricupsid valve regurgitation velocities.
An in-house lungworm (IDEXX angiodetect) test was run and this was positive for lungworm.
Treatment:
Penny was started on fenbendazole (Panacur) at 50mg/kg P.O. for 10 days for treatment of angiostrongylus. Prednisolone (Prednicare) 0.5mg/kg P.O. twice daily for 5 days then once daily was started to reduce inflammation. She was also started on sildenafil 1.2mg/kg P.O. for pulmonary hypertension.
Follow up:
At her recheck appointment Penny was doing very well. Her clinical signs had resolved, she was bright, exercising well and showing no tachypnoea or dyspnoea at home. Her heart murmur had resolved, her heart rate normalised to 84 beats per minute and her respiratory rate was normal at 32 breaths per minute. She was placed onto lungworm preventatives (Nexgard Spectra) given once a month. We are pleased to report that Penny continues to do well and has not required any long-term medication.
Discussion:
Penny threw up a few red herrings during her initial presentation and assessment. We hadn’t seen Penny for a few years, so it was unclear how long the heart murmur had been present. The numerous B-lines with a borderline left atrial size at initial presentation raised concerns over left sided congestive heart failure, and given her breed, thought to be due to mitral valve disease. She responded well to an initial treatment course for congestive heart failure.
On clinical examination a loud, right sided heart murmur was found- this raised a red flag to me. Mitral valve disease would give a predominantly left sided murmur. Review of her x-rays confirmed more right sided enlargement and a mixed pulmonary pattern which raised concerns over a primary pulmonary condition. Additionally, she was not up to date with her anthelmintic prevention which raised a concern over lungworm.
Her echocardiography supported pulmonary hypertension (PH). Differentials for PH include (Kellihan and Stepien, 2010):
- Secondary to left sided heart disease or congenital shunts
- Pulmonary hypertension secondary to respiratory disease, hypoxia or both
- Pulmonary emboli/thrombi/thromboemboli (PE/PT/PTE)
- Parasitic disease (Dirofilaria or Angiostrongylus infection)
- PH with multifactorial or unclear mechanisms e.g. masses
- Idiopathic
A positive Angiodetect (IDEXX) along with compatible clinical signs and echocardiography findings confirmed Angiostrongylus Vasorum with secondary pulmonary hypertension. This carries a very different treatment plan and prognosis to myxomatous mitral valve disease and congestive heart failure. We are very happy that Penny has made a full recovery and does not require long term heart medications.
Reference:
Heidi B. Kellihan and Rebecca L. Stepien (2010): Pulmonary Hypertension in Dogs: Diagnosis and Therapy, Vet Clin Small Anim, 40, pp 623-641